Alzheimer Brain Scans
Amyloid PET Scans for Alzheimer's Disease

In June 2012 Precision Imaging was the first radiology center in Maryland to offer and perform a β-amyloid brain PET scan with the newly-approved radiopharmaceutical Amyvid. The Amyvid scan was the first FDA approved in vivo test for the detection of the β-amyloid plaques that are deposited in the brains of patients suffering from Alzheimer's disease. The FDA has subsequently approved two other PET scans for the detection of β-amyloid plaques: Neuraceq in 2014 and Vizamyl in 2013. At Precision Imaging we use the Amyvid and Neuraceq PET scans.

The introduction of the Amyloid PET scan is an important breakthrough in the detection of Alzheimer's disease. Studies show that Amyvid is likely to detect the presence of β-amyloid plaques in the brain earlier and more accurately than any other brain imaging study —even before the patient develops any symptoms of Alzheimer's disease! Early and accurate diagnosis will be important in clinical efforts at slowing down the progression of this disease, and eventually in developing an effective treatment.
Why Choose Precision Imaging?
In June 2012 Precision Imaging performed the first clinical Amyvid brain PET scan in the state of Maryland. This "first" for Precision Imaging reflects our determination to pursue cutting-edge medical technology and bring it to clinical practice --right here, locally, in Montgomery county, Maryland.
As part of our involvement in medical research studies on Alzheimer's Disease and our clinical practice serving patients in our community, we have performed many amyloid brain PET scans with the radiotracers AV-45 (florbetapir), which became Amyvid, and now also Neuraceq (florbetaben). Florbetapir was acquired by the Eli Lilly pharmaceutical company in 2010, and was soon after approved by the FDA for clinical use in patients under the trade name Amyvid. Amyvid and Neuraceq are the two main FDA-approved studies for in-vivo detection of β-amyloid neuritic plaques in the brain --one of the hallmarks of Alzheimer's Disease.
At Precision Imaging, we leverage our extensive background in all aspects of neuroimaging including MRI and CT, our long experience with nuclear medicine brain SPECT and PET scans, and our seven-year hands-on work with these recently-approved brain radiotracers, to bring unmatched knowledge and quality service to our patients.
Why settle for service from a center that is just learning to perform β-amyloid brain imaging? Choose the experts at Precision Imaging!
At Precision Imaging, we understand our patients' need for privacy and confidentiality, especially in regards to an exam investigating the possibility of Alzheimer's disease. Under our care, your peace of mind includes the knowledge that your health information will remain confidential and secure. Talk to us about additional ways to ensure confidentiality of your health information.
Call us today for more information and to schedule an Amyloid Brain PET scan.
Alzheimer's Disease and the Value of the Amyloid Brain Scan
Alzheimer's Disease is a common disorder affecting the human brain. Symptoms include memory loss, confusion, language problems, personality changes, and difficulty understanding spatial relationships. The disease process begins decades before any symptoms develop. Eventually, enough nerve cells in the brain are damaged by the disease and are lost, resulting in impaired brain function which causes the classic symptoms of Alzheimer's disease. This disorder typically progresses unchecked, resulting in dementia, and eventually death.
One of the roadblocks to treating patients with Alzheimer's disease has been the difficulty in identifying people with this disorder early enough in the disease process, before there has been widespread nerve cell loss and irreversible symptoms. Also, many other disorders can cause memory loss, making it difficult to distinguish persons with early Alzheimer's disease from those with other conditions, thus hindering the study of early interventions to slow down the disease, and of new treatments to cure or stop it.
The introduction of the Amyvid and Neuraceq brain scans is an important breakthrough in the early detection of Alzheimer's disease. Studies show that these scans can detect the presence of the β-amyloid plaques at the heart of the disease earlier and more accurately than any other brain imaging study —even before the patient develops any symptoms of Alzheimer's disease!
A normal Amyvid scan can bring peace of mind.
An Amyvid scan showing evidence of early Alzheimer's disease can buy patients and their doctors a chance to pursue simple interventions such as certain healthy lifestyle changes, and to aggressively treat other conditions which enhance the progression of Alzheimer's, all while still early in the disease process. It affords them the opportunity to seek appropriate clinical trials of new medications currently in the research pipeline. It also allows patients and their families a chance to plan for the future. Early and accurate diagnosis of the Alzheimer's disease process with an Amyloid Brain PET scan will be an important tool in clinical efforts at slowing down the progression of this disease, in developing effective treatments, and eventually in developing a cure.
Call us today for more information and to schedule an Amyloid Brain PET scan.
Brain Amyloid Imaging for Alzheimer's Disease
Frequently Asked Questions
- What is Alzheimer's Disease (AD)?
- What is Mild Cognitive Impairment?
- How is AD diagnosed?
- What is the role of β-amyloid in the development of AD?
- What role does amyloid imaging play in the diagnosis and management of AD?
- Are there any treatments for AD?
- What are current uses for Amyvid scans?
-
What is Alzheimer's Disease?
-
Alzheimer's disease (AD) is a progressive, degenerative disorder affecting the brain. In AD the
nerve cells in the brain (neurons) are progressively damaged and eventually destroyed, resulting
in memory loss, problems with thinking and language skills, and behavioral changes.
AD
is not a normal part of aging, it is a disease
. AD is the most common form of dementia,
accounting for about 70% percent of all dementias. Symptoms usually develop slowly and
worsen over time, eventually becoming severe enough to interfere with daily tasks, with the
ability to carry on a conversation, and finally, affected persons are rendered unable to respond
to their environment. AD is the sixth leading cause of death in the United States. Patients with
AD usually live an average of 7 to 10 years after their diagnosis, but this can vary significantly
depending on patient's age at the time of diagnosis and presence of other diseases. Although the
greatest risk factor for AD is advancing age --most people with the disease are 65 years or older
--5% of patients develop early onset AD beginning in their 50s or even 40s.
-
Alzheimer's disease (AD) is a progressive, degenerative disorder affecting the brain. In AD the
nerve cells in the brain (neurons) are progressively damaged and eventually destroyed, resulting
in memory loss, problems with thinking and language skills, and behavioral changes.
AD
is not a normal part of aging, it is a disease
. AD is the most common form of dementia,
accounting for about 70% percent of all dementias. Symptoms usually develop slowly and
worsen over time, eventually becoming severe enough to interfere with daily tasks, with the
ability to carry on a conversation, and finally, affected persons are rendered unable to respond
to their environment. AD is the sixth leading cause of death in the United States. Patients with
AD usually live an average of 7 to 10 years after their diagnosis, but this can vary significantly
depending on patient's age at the time of diagnosis and presence of other diseases. Although the
greatest risk factor for AD is advancing age --most people with the disease are 65 years or older
--5% of patients develop early onset AD beginning in their 50s or even 40s.
-
What is Mild Cognitive Impairment?
-
Mild cognitive impairment (MCI) is a slight but noticeable and measurable decline in a person's cognitive
abilities, including memory, reasoning, and other thinking skills. A person with MCI is at a significantly
increased risk of developing full-fledged Alzheimer's Disease or another dementia. In some people, MCI
may represent an early stage of the disease process that eventually leads to clinical AD. Therefore,
persons with MCI are good candidates for Alzheimer screening, in the hope of diagnosing the disease process
early enough to try to intervene and modify this process.
-
Mild cognitive impairment (MCI) is a slight but noticeable and measurable decline in a person's cognitive
abilities, including memory, reasoning, and other thinking skills. A person with MCI is at a significantly
increased risk of developing full-fledged Alzheimer's Disease or another dementia. In some people, MCI
may represent an early stage of the disease process that eventually leads to clinical AD. Therefore,
persons with MCI are good candidates for Alzheimer screening, in the hope of diagnosing the disease process
early enough to try to intervene and modify this process.
-
How is AD diagnosed?
- Other causes of cognitive impairment must first be looked for and ruled-out, such as adverse effects of medications, hormonal problems, vitamin B12 deficiency, normal pressure hydrocephalus, chronic brain hypoxia, intracranial bleeding, and other neurodegenerative diseases. This is why a check-up with a doctor is a necessary first step in the work-up of someone for possible AD.
- A clinical diagnosis of AD requires the presence of dementia (cognitive impairment of sufficient severity to prevent independent function by the patient). Clinical diagnosis is therefore not able to diagnose the disease process early, and is only moderately accurate: wrongly diagnosing AD as being present 30% of the time (70% specificity) and not diagnosing it when it is present 15-20% of the time (sensitivity 80-85%).
-
Specific biomarkers for Alzheimer's-related pathology, such as β-amyloid plaques
diagnosed on amyloid imaging studies, can allow for earlier and more accurate diagnosis of
the Alzheimer's disease process, while the symptoms are still mild or even absent.
-
What is the role of β-amyloid in the development of AD?
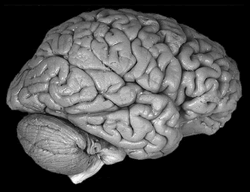
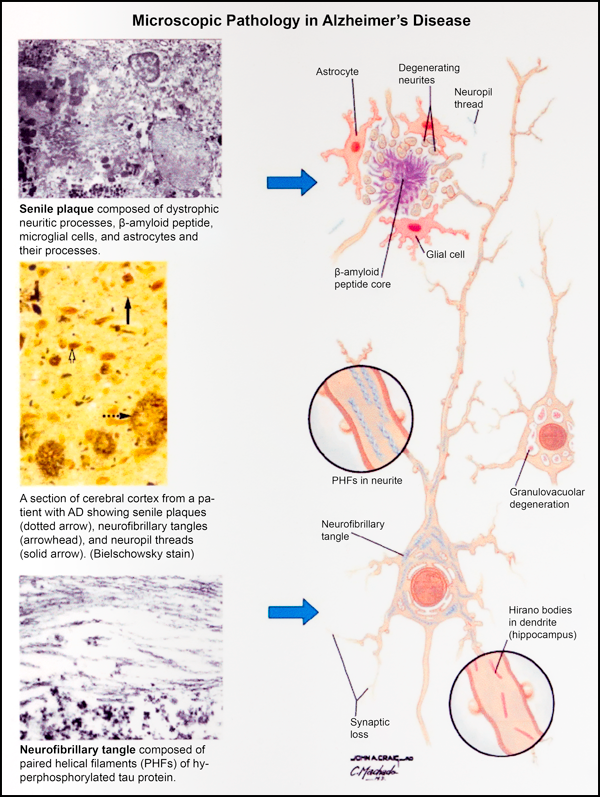
- β-amyloid plaques are present in significant numbers in the cortex (surface grey matter) of the brain in all cases of AD. These β-amyloid plaques develop many years before the onset of dementia. When these plaques are associated with damage of nearby neurons and inflammation they are described as "neuritic plaques". Dense neuritic plaques, together with the microscopic brain lesions called "neurofibrillary tangles", are the hallmark of AD, necessary for a pathologic diagnosis of AD.
- Not only are neuritic β-amyloid plaques always present in the brains of persons with AD, most brain researchers now believe that these plaques are actually involved in causing the disease. Mutations of genes involved in the handling of brain β-amyloid particles have been found in persons suffering from familial early-onset AD and in those suffering from sporadic late-onset AD. These β-amyloid mutations are involved either in the production or the removal of β-amyloid from the brain, resulting in increased accumulation of β-amyloid particles in the brain.
-
When the handling of the β-amyloid particles is disturbed (either by genetic, acquired
or environmental factors, or more likely by a combination of factors) such that the particles
begin to accumulate, they tend to aggregate into insoluble polymers that become the β-amyloid
plaques. Many processes have been proposed to explain how the β-amyloid plaques
damage and eventually kill the neurons of the brain, and the exact mechanisms remain controversial.
This is an active area of brain research and many scientists believe that targeting these
mechanisms may someday lead to effective treatments for AD.
Back to Top. -
What role does amyloid imaging play in the diagnosis and management of AD?
-
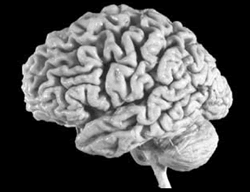
CT, MRI, and FDG-PET scans of the brain have been used to help in the diagnosis of AD.
- CT and MRI scans are generally very useful tests and just about everyone being evaluated for AD should have one of these studies to assess the overall health of the brain tissue. But when looking specifically for AD, CT and MRI rely on finding structural changes in the brain, especially looking for shrinking volumes in certain regions of the brain that are typically affected by the disease. Unfortunately, many other conditions also shrink the volumes in these regions of the brain and therefore these structural scans can only seldom tell patients with AD apart from other patients, or even from healthy age-matched persons!
- FDG-PET scans measure the accumulation of an injected, sugar-like substance within the brain. These scans look for areas of the brain that have been sufficiently affected by the AD process that they no longer function normally, sometimes even before they show significant volume shrinkage on CT or MRI. A specific pattern of affected brain regions on an FDG-PET scan strongly supports a diagnosis of AD. FDG-PET scans can often tell affected individuals from healthy persons 5 to 10 years before the onset of clinical AD.
-
CT, MRI, and FDG-PET scans of the brain have been used to help in the diagnosis of AD.
-
Amyvid scans have recently been approved for clinical use by the FDA, and show promise of diagnosing the
AD process earlier and more accurately than other types of scans.
- Amyloid brain scans use the same PET machines as in the FDG-PET scans, but a different tracer is injected.
-
Instead of looking for regions of malfunctioning brain tissue, Amyvid scans look for abnormal
deposits of the β-amyloid particles in neuritic plaques within the brain, possibly finding
these areas before the development of abnormal function (FDG-PET) or volume shrinkage (CT and MRI).
Amyloid brain scans can often tell affected individuals from healthy persons 15 to 20 years before
the onset of clinical AD.
-
Are there any treatments for AD?
-
Unfortunately, at present there is no proven effective treatment for AD, only modestly effective
medications for relieving some of the disease's symptoms. However, there is a growing demand for
earlier diagnosis of Alzheimer's pathology:
- Patients and their families are demanding prognostic information for family decision-making and financial planning.
- Medical researchers want to test new therapies for AD earlier in the course of the disease process, before the development of dementia, when the treatments are more likely to alter the course of the disease and to benefit the patients.
- Amyloid imaging is also contributing to the development of AD therapies by allowing better selection of patients for clinical trials and by providing a non-invasive way of assessing the effect of these therapies on the brain's amyloid load.
-
Unfortunately, at present there is no proven effective treatment for AD, only modestly effective
medications for relieving some of the disease's symptoms. However, there is a growing demand for
earlier diagnosis of Alzheimer's pathology:
-
What are current uses for Amyvid scans?
- Confirmation or exclusion of AD.
- Earlier diagnosis of AD or probable AD.
- Telling different dementias apart, especially AD vs. frontotemporal dementia, since they must be managed differently.
- Diagnosis of AD or probable AD in cases of other inconclusive scans.
-
Adjunct to medical research for AD, including clinical trials.
Amyvid Case Studies
At Precision Imaging we have been performing β-amyloid brain PET scans for more than seven years, initially as part of research studies on patients with Alzheimer's disease and also, since June 2012, as routine clinical studies on non-research patients. We have thus gained a great deal of experience performing and interpreting Amyvid scans. Here are some recent case studies from our imaging center demonstrating the usefulness of this new study.
Case 1 Case 2 Case 3
Case 1
63 year-old male complaining of increasing difficulty with the cognitive aspects of his high-level financial industry job. A recent MRI, performed at another imaging center, was read as "normal".
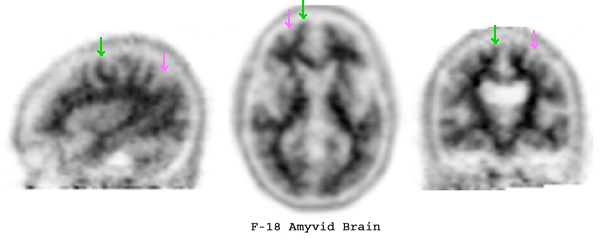
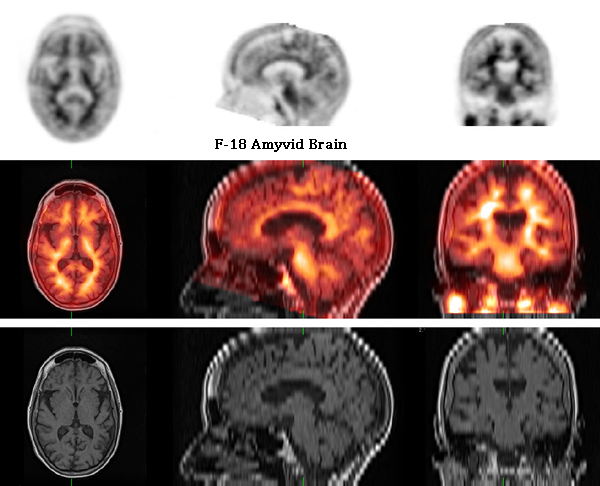
These three representative Images from the Amyvid PET scan demonstrate normal uptake of the radiotracer in the white matter of the brain (green arrows) and no significant uptake in the grey matter (pink arrows). This is a negative study, indicating that there is no significant neuritic plaque formation in the brain (the presence of neuritic plaques is a hallmark of Alzheimer's disease).
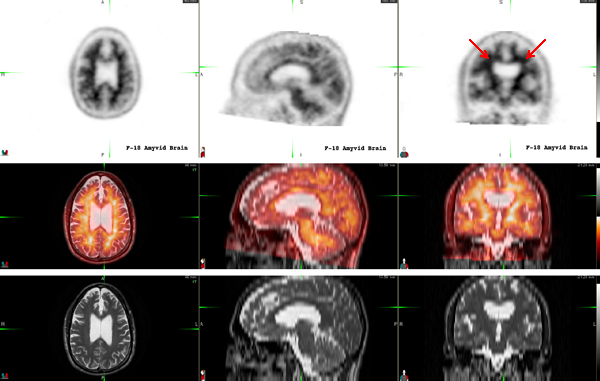
We requested the recent outside brain MRI and fused it on a computer with the our Amyvid PET scan. This helps to confirm that the uptake of Amyvid is exclusively in the white matter and spares the grey matter.
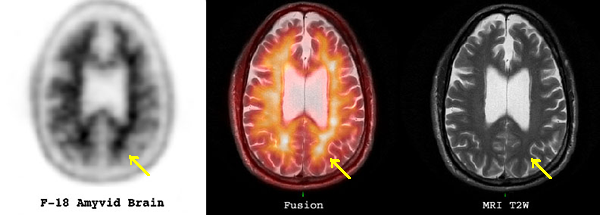
The value of the MRI fusion can be shown in this transverse slice through the upper part of the brain. There is asymmetric Amyvid uptake in the left occipital region (left image, yellow arrow), that could be easily confused with accumulation in the cortex of the brain and which could have been misinterpreted as the presence of neuritic plaques in this region of the brain. The corresponding PET-MRI fusion image shows that this represents normal uptake in an area of asymmetric white matter (middle image, yellow arrow), with no grey matter present in this location (right image, yellow arrow). This is therefore a normal scan.
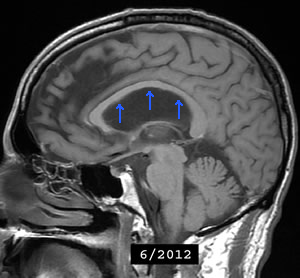
Finally, as a value-added part of a scan at Precision Imaging, we noticed that the ventricles of the brain seemed too large on the coronal sections (red arrows, fusion image group). We reviewed the MRI from the outside imaging center and found that the white matter structure called the corpus callosum was somewhat thin and bowed upwards on the sagittal sections (blue arrows), and we therefore suggested that early normal pressure hydrocephalus may be present and could be contributing to the patient's symptoms. Normal pressure hydrocephalus is a relatively common, treatable, cause of cognitive impairment. The patient was referred for further workup of possible hydrocephalus.
One of the important teaching points this case highlights is the clinical impact that a negative Amyvid study can have on patient management. Even if the outside MRI had been correctly interpreted as showing possible early hydrocephalus, the confirmatory tests are invasive and the treatment is neurosurgical, neither of which would be vigorously pursued if the patient suffered from Alzheimer's disease. This negative Amyvid scan gave the patient and his physicians confidence to workup and, if present, to aggressively treat the normal pressure hydrocephalus.
Case 2
75 year-old female with dementia. A recent MRI was negative.
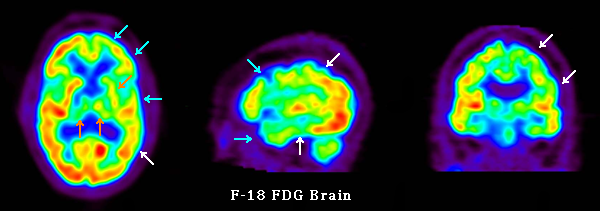
An FDG-PET scan of the brain was performed showing indeterminate findings: reduced metabolism in the temporoparietal regions, especially on the left side, suggesting Alzheimer's disease (white arrows); reduced metabolism in the frontal and anterior temporal regions, also mostly on the left, suggesting frontotemporal dementia (blue arrows); and reduced metabolism in the thalami and left basal ganglia suggesting multi-infarct dementia or other cerebrovascular disease (orange arrows).
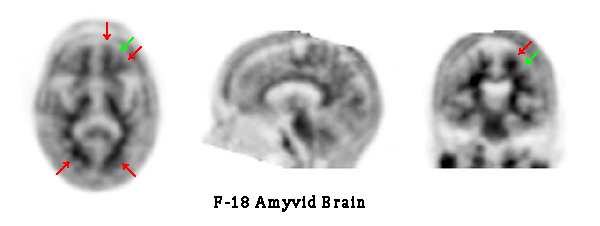
An Amyvid PET scan was then performed in order to clarify the nature of the dementia. The Amyvid scan shows normal radiotracer uptake throughout the white matter of the brain (red arrows) and no significant uptake in the cortex (white arrows). In our experience, for an older patient with dementia, this scan essentially rules-out Alzheimer's disease.
The recent MRI scan was fused to the Amyvid PET scan, confirming that the radiotracer uptake was confined to the white matter tracts. Since there is only mild cortical atrophy in this particular case, the Amyvid-MRI fusion was not as crucial in making the diagnosis. However, in cases where there is significant brain atrophy, with thinning of the cortical grey matter, the fusion Images can be invaluable in determining the exact distribution of the radiotracer. Subsequent genetic testing (a positive GRN mutation) conclusively diagnosed frontotemporal dementia.
This case highlights another important teaching point: the value of an accurate diagnosis. Before the Amyvid
scan was performed, Alzheimer's disease was the most likely clinical diagnosis. However, cholinesterase inhibitors
(Aricept, Exelon, Reminyl), which are currently the mainstays of symptomatic treatment for Alzheimer's disease, are
contraindicated in cases of frontotemporal dementia and may even make the patient's symptoms worse. Witout the
Amyvid scan the patient would have almpst certainly received a wrong treatment which likely would have worsened
her condition.
Case 3
68 year-old male with cognitive impairment, a mini mental status exam of 24/30, and a history of concussions at a younger age. PSA levels are elevated, raising the possibility of prostate cancer, not yet worked-up.
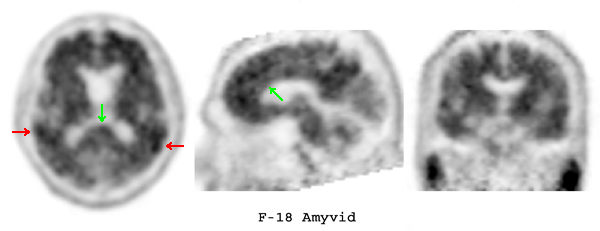
An Amyvid PET scan showed significant radiotracer uptake throughout the cortex of the brain, in addition to the expected normal uptake in the white matter tracts. Indeed, cortical radiotracer uptake in parts of the temporal lobes (red arrows) have greater Amyvid accumulation than does the white matter (green arrows). This Amyvid scan is positive, indicating the presence of significant β-amyloid-containing neuritic plaques in the cortex of the brain, and in our experience, is virtually diagnostic of Alzheimer's disease.
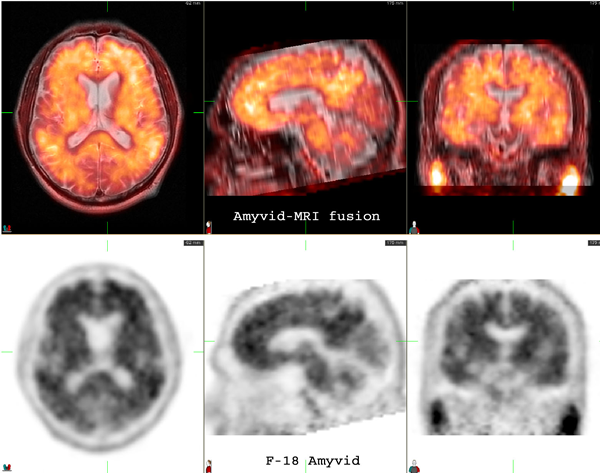
An outside MRI scan was fused to the Amyvid PET scan, confirming that the radiotracer uptake is diffusely present in the cortex of both hemispheres of the brain.
This case highlights one of the values of a positive Amyvid scan: The patient can still be worked-up for possible prostate cancer. But if this diagnosis is confirmed, the aggressiveness of the treatment will be tempered by the diagnosis of Alzheimer's disease confirmed by Amyvid PET.